As 2024 approaches in the United Kingdom, a healthcare sector at once lost and facing new challenges attempts to find its way again. The potential inflection point is upon us, and this formative year will determine what survives in its prior state against that which crumples under pressure; the years of complete generational change on our threshold remind me to expect creative problem-solving as we head towards greater harmony.
The Triple Threat: A Perfect Storm
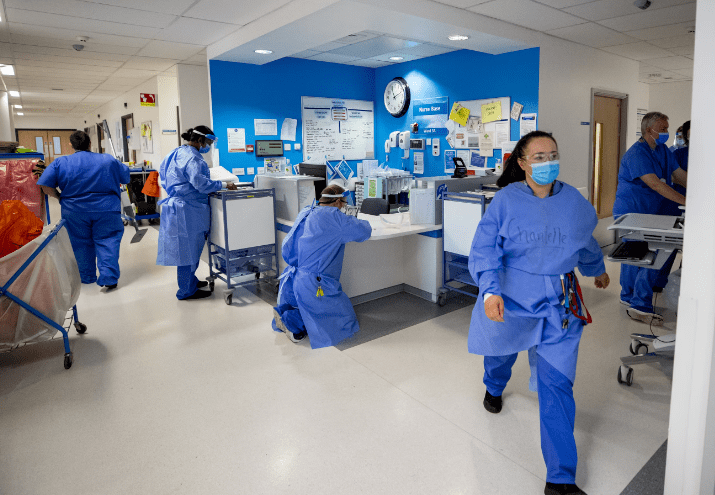
In a perfect storm of converging pressures facing the healthcare system in 2024, Overwhelming demand, a growing populace of elderly people and the inescapable clamp of inflation has conspired to stretch both National Health Service (NHS) and social care services on the rack. The effects of this bottleneck are felt throughout the healthcare environment, with longer waiting lists and developments created by work constraints.
Rising Concerns on Waiting Lists
With the dawn of a new year, such an approach would quickly come up against the crippling elective care backlog that has formed in NHS. These figures bear testimony to the capacity challenges our health system is struggling with over recent months, as evidenced by a record-high number of 7.8 million people waiting for hospital treatment in September this year. Taking all of this into account, the backlog has decreased marginally down to 7.6 million as at April 2034 yet it is undeniable that numbers have a long way further urging given its depth and size.
It was the classic vicious circle of delayed discharge.
This healthcare system bottleneck is not limited to the walls of hospitals as we also see significant pressures being applied in delayed discharges. Figures compiled by NHS England have shown that earlier this year some 13,200 to 14,200 patients who were well enough to leave hospital stayed in a bed every day last month. But this is a shocking 1 in every 8 or so general and acute beds currently asensolging resources away from patients in hospitals up along England which illustrates the enormous opportunity cost of delayed discharges on hospital performance (and patient care).
Support Services for Social Media: The Mental Health Cries
Physicians should not think that they have a duty to fix all the ailments of patients, for the challenges with healthcare are more than just physical. At the same time, mental health services have also faced challenges as demand increases but capacity remains constrained leading to long waiting times and few options for care. This gap clearly demonstrates a need for comprehensive care that deals with the mental and physical aspects of health, urgently.

The Bedrock of Primary Care
The pressure on hospitals is not limited to PCUs — but elsewhere in healthcare, both GPs and dentists are struggling because of their spare capacity. Delays in waiting for appointments have recently become the norm, which only adds to the stresses being put on this system and highlights a significant role needing played with respect building up primary care services.
The Intractable Problem of the Labour Force
A more than 20-year worker shortage crisis looms directly in the center of this capacity issue. Fig 1: Permanent NHS workforce in England, and long term trends Source: Authors’ calculations based on data from the UK Labour Market Report (ONS)The sobering message of the NHS Long Term Workforce Plan for England released June was that getting a handle on such scaling issues will require almost two thirds more permanent employees in the health services than when it had over 1. This figure is alarming and it underlines the urgent requirement for strong workforce planning and proactive recruitment of healthcare workers.
Fill In The Blank: Trapped When Complaints Strike Back
With a historic six-day junior doctor strike kicking off the year 2024, it was clear there were widespread issues simmering within the health workforce. This dual front of a simmering dispute over pay and working conditions, combined with the threat of further stoppages potentially pushing an already creaking healthcare system to breaking point.
Save the Attached Regulatory Reforms to Protect Patients
Following shocking news of the actions of Lucy Letby, who has been convicted now you’ll be pleased to hear that she will hopefully never hold any type of position whereby lone working is necessary around defenceless patients again and central government have stepped in promising action on NHS managers. This reform in regulation is intended to strengthen patient safety and hold the healthcare system more accountable, an essential part of rebuilding public confidence in oversight that maintains the highest possible standards for care.
The Delicate Balance of Migration Debates
The government is preparing to face pressure on migration as it wrestles with how the levelling up agenda can be reconciled with severe workforce shortages in key sectors such as social care without numbers of new arrivals. Abstract Finding the fragile balance between policy goals and ground-level detail will be a key test with implications that extend across the healthcare workforce, as well as quality of care.

Tactics for endurance: The means ahead
The government and healthcare authorities are considering the strategies to strengthen the capacity of health system on how we can improve it moving forward.
Investing in Infrastructure: Expanding the Capacity
Realizing the pressing need to increase capacity, the government has proposed investing in next of modern IT systems, medical equipment and upgrading infrastructure. This includes £3.4bn allocated for digital technology and equipment in the March 2024 Budget, which is intended to make the NHS more productive while increasing efficiency.
Moving from Medical Care to Community Care
There is a growing consensus among more diverse political stakeholders that care should be arranged to or moved from the hospital setting in favour of community-based delivery. The goal of this paradigm shift is to offer more individualized, coordinated and convenient care that responds better to the unique needs of each person. Pharmacy-led interventions including community pharmacy services and integrated primary care are likely to be key drivers in this shift.
Preventative Health Measures: 1 Ounce of Preclusion
The old saying is still very much true: an ounce of prevention, etc. Podcasting gives our customers that seamless integration for both the small tasks and bigger ones — they collectively have a tremendous influence on your deployment time Verification Time would be reduced by listening to this Both sides of politics have agreed in principle about the need to reduce pressure on hospitals through preventative health measures. There is some promise that the health of people could be improved, and healthcare services relieved from a substantial burden by initiatives such as those announced last week for tobacco control (introduction of phasing out cigarettes over time) relative to non-health benefits in addressing major causes leading to ill health but accounting for most deaths.

Integration and Collaboration: Blinds are broken by toughest silos
Bearing in mind the reciprocal relationship between health and social care services, future governments are expected to implement further measures aimed at better integration of these sectors more broadly. In June 2022, 42 integrated care systems were officially launched in England to join up health and social care providers as they work together across primary and acute settings to provide more coordinated support for patients during their visits.
The Challenge with Digital Transformation and Embracing Innovation
With digitization acting as the impetus to achieve improved efficiency and outcomes, the healthcare industry thrives on embracing digital transformation. Following roll-out, it is anticipated that initiatives such as expanded use of digital care records and virtual wards will help to create end-to-end processes supported by shared information between providers -ultimately helping better share capacity across sites.
A New Dawn For Life Sciences Advancements
Life science has even greater potential to revolutionize global health outcomes on a wider scale beyond the region of UK. The 2024 launch of malaria vaccines is a huge leap in the halting of this disease that kills over half a million people worldwide each year. On a more domestic front, as the life sciences community looks at biomedical options for its future health and associated healthcare privacy challenges have an optimistic agreement on access to medicines & plans to boost uptake of drugs offered new hope encouraging innovation.
The Road Ahead: Navigating a Path of Uncertainty Through Resilience
In the troubled times of 2024, we provide continued and relentless support to an NHS on a treadmill that has finally hit warp speed but also redemption lies in their resolve for unity as five diverse nations; this our bond toward sustainability. The general election will provide a platform to resolve some of these issues, with debates on healthcare productivity, immigration and access to care set for the campaign basement.
However, no matter how rocky the ride ahead will be, one thing is for certain — it will rely on the strength and resolve of healthcare workers who are dedicated to their mission as well focusing on a new path through innovation and collaboration in order to create future state that finally this time more equitable.
The UK’s healthcare landscape is on the cusp of a new era, as it weathers its way through this ordeal that promises to put our systems under strain and shape how once unprecedented changes may forge more systemic shifts towards an equitable society where citizens’ matters — their welfare in health care terms without exception.